#SjekkDeg: The campaign that’s getting Norwegian women screened

Photo credit: Jorunn Valle Nilsen
Every January, Norway launches the #SjekkDeg campaign, a nationwide initiative aimed at increasing awareness about cervical cancer and encouraging women to participate in regular cervical cancer screening. The name, which translates to “#CheckYourself,” is a clear and compelling call to action. Since its inception, #SjekkDeg has played a crucial role in informing the public and increasing participation in the Norwegian Cervical Cancer Screening Program.
The origins of #SjekkDeg: A personal story driving public action
The #SjekkDeg campaign was established in 2015, by Thea Steen, a 26-year-old Norwegian journalist diagnosed with cervical cancer. Rather than keeping her struggle private, Thea shared her experience publicly, urging other women to attend regular screenings. Her powerful message gained national attention and motivated the Norwegian Cancer Society and Cancer Registry of Norway to formalise the #SjekkDeg campaign. Today, it stands as a testament to how personal storytelling can drive public health outcomes.

Marketing strategies and public engagement
The success of the #SjekkDeg campaign relies heavily on effective communication and public engagement. Each year, the campaign employs a multi-channel marketing strategy to reach a broad audience and encourage participation. Key components of the marketing strategy include:
- – Social media: Social media platforms like Instagram and Facebook play a pivotal role in the campaign’s outreach. By sharing real-life testimonials, video messages from healthcare professionals, and engaging content from influencers, the campaign reduces stigma and makes the conversation around cervical cancer approachable. The use of the hashtag #SjekkDeg helps build a recognizable digital footprint and fosters community engagement.
- – Collaborations with media: National and regional media outlets play a vital role in spreading the message. Interviews, feature stories, and opinion pieces highlight the importance of cervical screening and share personal experiences from women who have benefited from early detection.
- – Targeted messaging: The campaign uses targeted messaging to address specific demographic groups. For instance, younger women may receive digital reminders and information through social media, while older populations are reached through traditional media and direct mail campaigns.
- – Integrating healthcare providers: General practitioners, gynaecologists, and public health clinics are crucial partners in the #SjekkDeg campaign. They provide patients with information, encourage participation, and offer free or very cheap accessible screening appointments.
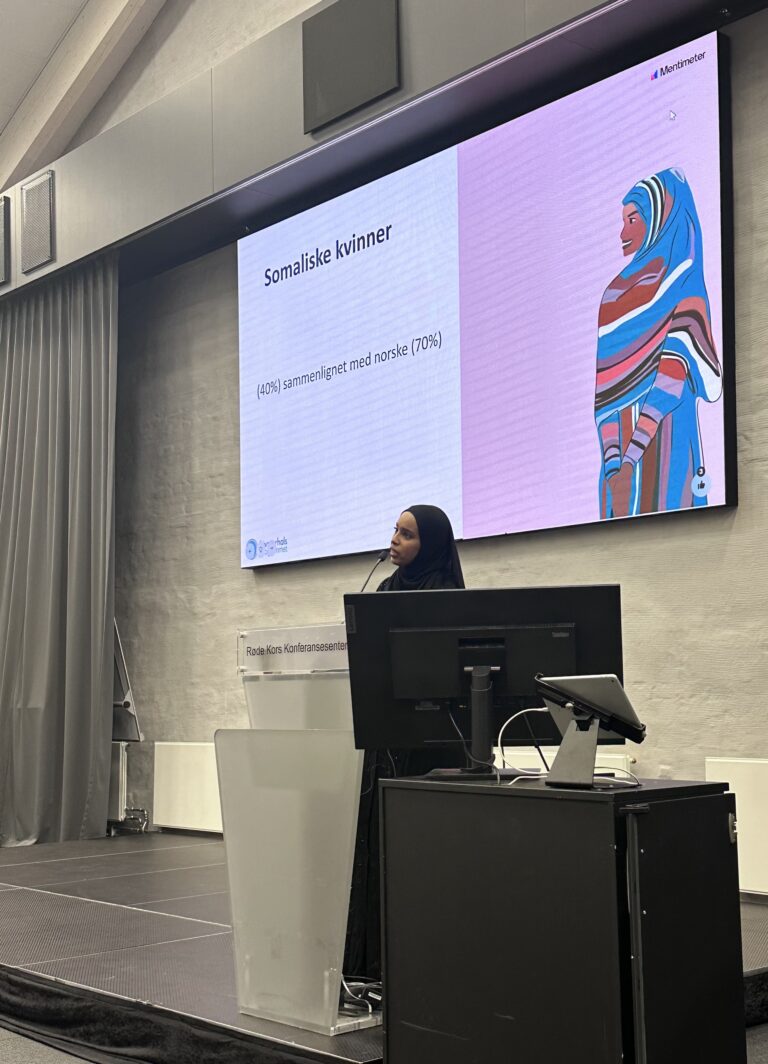
- – Community events and grassroots activation: Throughout the campaign in January, local communities organise local events, public talks, and free screening opportunities. By engaging with communities in familiar environments, #SjekkDeg lowers practical and psychological barriers to participation. These face-to-face initiatives create a tangible connection to the campaign’s mission.
- – Sharing screening data: The Cancer Registry shares updated data on screening participation and lives saved with the Norwegian Cancer Society and the media. By showcasing these results, the campaign not only motivates more women to get screened but also strengthens the case for increased funding and resources. Demonstrating the campaign’s impact encourages policymakers and stakeholders to invest more in future outreach efforts.
- – Invitation letters: During the campaign, CervicalScreen Norway sends invitation letters to 25-year-olds, welcoming them to the screening program for the first time. This targeted outreach ensures young women understand the importance of regular cervical screening from the start.
- – Avoiding cultural barriers: By running the campaign in January, #SjekkDeg strategically avoids overlapping with Ramadan, ensuring that women from diverse cultural backgrounds can participate in screenings without conflict.

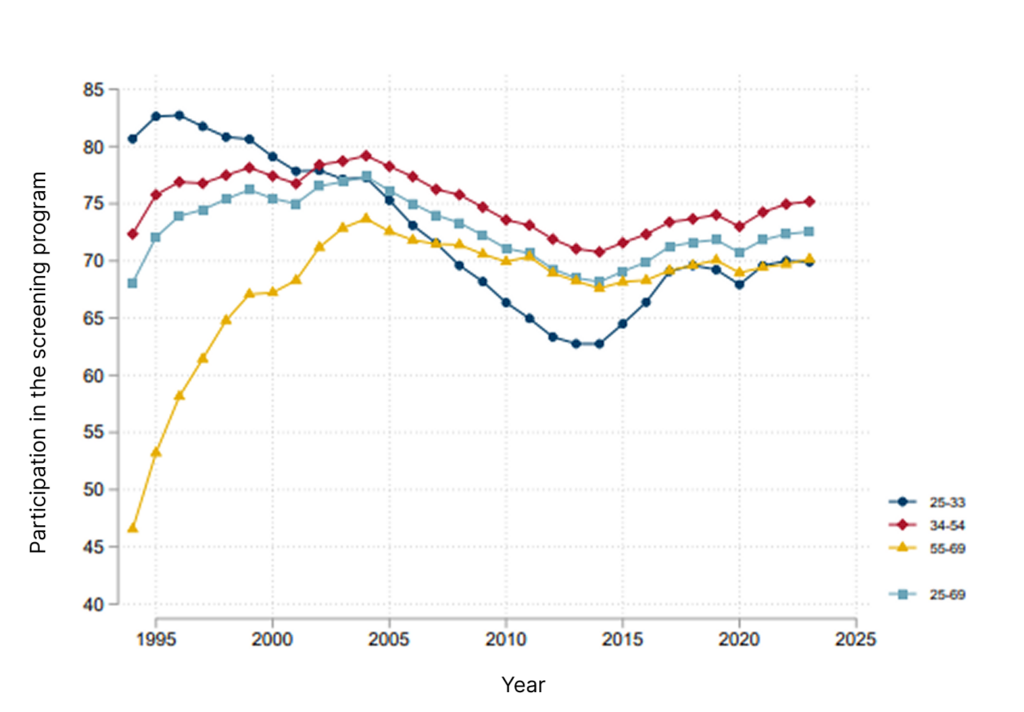
Measuring impact
Since its launch in 2015, the #SjekkDeg campaign has contributed to a significant increase in cervical cancer screening participation rates in Norway. Thousands of women have undergone screening as a direct result of the campaign’s efforts, leading to the early detection of precancerous conditions and a reduction in cervical cancer cases.
Inspiration for cancer screening campaigns
The #SjekkDeg model provides key insights for anyone planning similar campaigns:
- – Humanize the message: Personal stories, like Thea Steen’s, break through apathy and create emotional connections that drive behaviour change.
- – Multi-channel approach: Combining digital, print, and in-person outreach ensures comprehensive coverage and reaches diverse audiences.
- – Partner with trusted voices: Collaboration with healthcare providers and media outlets enhances credibility and extends reach.
- – Adapt to cultural contexts: Tailoring communication to different age groups and cultural backgrounds increases engagement and accessibility.
Commercially available HPV assays used in screening detect 14 high-risk (hr) HPV genotypes. While HPV testing is more sensitive than cytology, detecting all 14 types together does not differentiate between transient infections and persistent infections that can lead to cancer.
When HPV-based screening was implemented in 2019, all hrHPV-positive women with abnormal cytology were referred for colposcopy and biopsy, leading to a 60% increase in colposcopy referrals. This created a suboptimal clinical management system with low predictive value, excessive use of health care services, and distress among women. DOI: 10.1158/1055-9965.EPI-22-0340
In our effort to calibrate the follow-up algorithm, we relied on the premise that each of the 14 distinct hr HPV genotypes possesses its own unique carcinogenic potential and cervical cancer risk profile. More than 3000 hrHPV positive women were assessed for risk of cervical precancers and cancers while separating the most carcinogenic genotypes, HPV16 and 18, from the pool of the remaining hrHPV types. DOI: 10.1038/s41416-020-0790-1
As a result, this new screening algorithm reduced unnecessary colposcopy referrals with biopsy for women with lower precancer or cancer risk. Based on our research, the follow-up algorithm for HPV-positives was changed in July 2018.
Ongoing research aims to develop more effective clinical algorithms for managing HPV-positive women. Our focus includes methylation markers, the combination of methylation and HPV genotyping, and the integration of methylation with cytology. Several studies are also evaluating the most suitable screening strategies for HPV-vaccinated populations. Additionally, research into risk-based screening seeks to optimise cancer prevention by tailoring follow-up strategies to individual risk profiles.
Insights for European screening programs
CervicalScreen Norway demonstrates how evidence-based strategies can enhance cervical cancer screening. The integration of HPV self-sampling has improved access, particularly for underserved groups, and research suggests that direct mailing of test kits could further boost participation.
Ongoing efforts focus on optimising risk-based screening, refining triage protocols for HPV-positive individuals, and tailoring strategies for HPV-vaccinated populations. By sharing our research and experiences, we aim to support European countries in strengthening their screening programs and advancing cervical cancer prevention.
Subscribe to our newsletter to get news and updates.
Subscribe to our newsletter to get news and updates.

The general objective of EUCanScreen is to assure sustainable implementation of high-quality screening for breast, cervical and colorectal cancers, as well as implementation of the recently recommended screening programs – for lung, prostate and gastric cancers. EUCanScreen will facilitate the reduction of cancer burden and achieving equity across the EU.
This project has received funding from the European Union’s EU4HEALTH Programme under the Grant Agreement no 101162959